Value-based Vascular Surgery
Learnings and ideas from a month on surgery rotations
Wishing everyone a happy Thanksgiving 🦃 weekend!
Have been heads down on a clinical rotations since I last wrote here, but wanted to take some time to share a few of the learnings I’ve had from the last month of my surgery rotation as a MS3. Spending time with surgery trainees, fellows, and attending surgeons have given me tremendous respect for the impact surgery has on patients and our healthcare system:
As demanding as the surgeon’s lifestyle is, it’s arguably one of the most rewarding and impactful ways to intercede for another human being. Few other specialties allow the same magnitude of impact on a patient’s quality of life: whether it’s removing a symptomatic gallbladder to transplanting a new kidney, almost every case I’ve scrubbed have been a significant life-extending (sometimes life-saving) procedures that lead to incredible gratitude. You get to see patients walking again without debilitating pain after a vascular angioplasty or knee replacement, gaining newfound strength and time after coming off energy-draining dialysis with a new kidney, and so much more.
The amount of trust patients place in the surgeon’s hands is tremendous. When the patient is on the operating table, their life becomes very much in the hands of the surgeon and the team in the operating room (OR)… but the trust starts way before they get to the OR - in the counseling and decision-making process to receive surgery, in thoroughly explaining the various complications (sometimes life-threatening complications) that can arise unexpectedly, in the tough conversations with patient’s holding out hope for a surgical Hail Mary that another surgery may not appropriate or ultimately beneficial.
At the health system level, surgery can ultimately be one of the most expensive interventions that we have as a last resort when more conservative or cost-effective management fails. However, when managed well post-operatively and triaged well pre-operatively…I’ve seen how surgery can be part of high-value care that provides the best care possible while still being resource-efficient.
Most of my time this month as a medical student has been with the vascular surgery service - a surgical specialty that treats conditions of the arterial, venous, or the lymphatic systems. Working with vascular surgeons in the operating room (OR) has shown me a variety of fascinating cases from aortic aneurysm repair, to angioplasties, to AV Fistula creations, to carotid endarterectomies. When I’m not in the OR I get to sharpen my preoperative and postoperative medical management of vascular surgery patients which involves rounding early in the mornings to change wound dressings and spending the afternoon working up postoperative complications like sepsis or even necrotizing fasciitis.
As a value-based care enthusiast, the conversations in surgery that were most interesting to me revolved around how surgeons decide when a surgical intervention is appropriate over conservative management (e.g., angioplasty vs supervised exercise therapy) and how vascular surgery intersects with other specialties (e.g., nephrology in the creation of AV Fistulas).
Vascular surgery is particularly interesting to consider in the context of specialty-based value-based care models because of how surgeons ultimately manage chronic conditions like peripheral artery disease (PAD), venous insufficiency, diabetic ulcers, and chronic kidney disease via arteriovenous fistula creation. I’ll touch on a few insights I gleaned over these past few weeks as I’ve taken some time to reflect on ways to integrate the acute and chronic aspects of vascular surgery.
Supervised exercise therapy as first-line treatment for PAD
One of the most common conditions I saw treated both in the operating room and managed in the outpatient environment was symptomatic peripheral artery disease - the classic patient vignette goes a little like this: 52 yo patient with past medical history most significant for smoking, hyperlipidemia, and hypertension presenting with pain (“claudication”) after 2 blocks of walking and occasionally pain at rest.
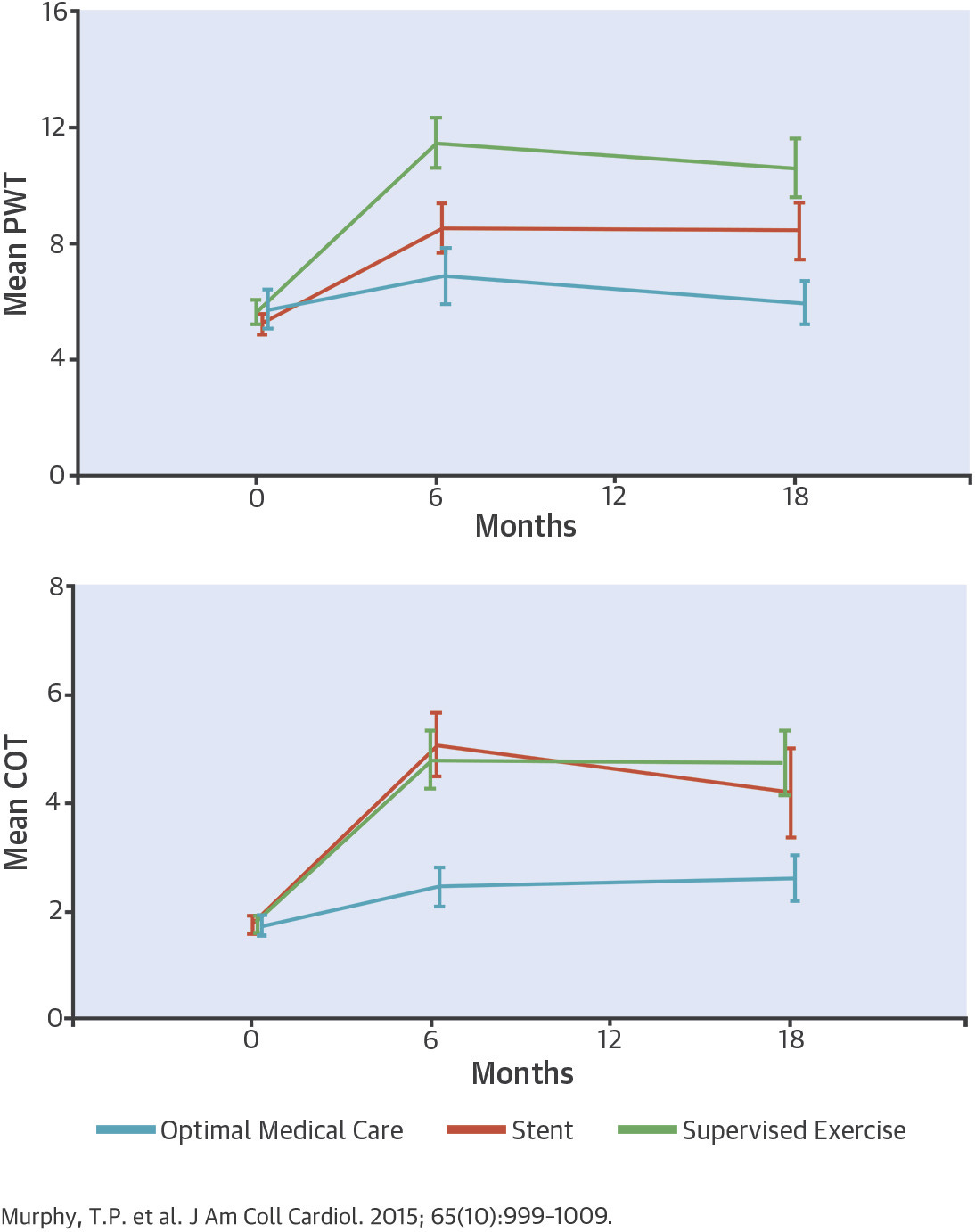
The CLEVER trial randomized symptomatic PAD patients into supervised exercise therapy, stenting, and optimal medical therapy (e.g., cholesterol reduction, antiplatelet therapy, blood pressure management) and found that exercise therapy provided comparable durable improvement in functional status and quality of life up to 18 months later. Further studies on cost-effectiveness in the Netherlands comparing exercise therapy vs endovascular repair showed that in a 5-year timeline, exercise therapy saved more than $7.2K per patient per year.
In addition, there is a rise in the trend of office-based vascular procedures that allow conditions like PAD to be managed in an outpatient vascular surgical practice. Studies show that outcomes remain comparable and help consolidate costs and create more flexibility for the surgeon and also can lead to better patient experiences without various service lines competing for constrained resources.
Though I remain skeptical how value-oriented these ambulatory surgery centers can be as these centers may be less accountable for unnecessary surgical interventions than larger hospital systems, the premise of more streamlined operations opens up an opportunity to consider what a population health-based approach to surgical management of vascular diseases may look like.
Post-surgical management and the Perioperative Surgical Home Model
A good deal of the time I spent on the surgery wards was helping the team manage perioperative recovery and medically optimizing patients for discharge. Today, many surgical specialties are measured directly around a patient’s operation like hospital length of stay (LOS), reducing post-surgical complications, and improving 30-day survival. Over time (and much policy reform) we may see a larger shift towards longer-term metrics like functional recovery and other patient-centered outcomes. To better support these value-based models, we may see incentives for more detailed preoperative screening to assess patients’ functional status at baseline and preoperative medical optimization to reduce overall readmissions and healthcare costs.
Evidence-based perioperative management like Enhanced Recovery After Surgery (ERAS) programs offer recommendations in fluid intake to avoid AKI (which can occur in >30% of post-cardiac surgery patients). Highlighting the perioperative surgical home (PSH) as one of the few ongoing experiments in coordinating team-based care around a surgical patient, consider a few of the differences between traditional and PSH shared-decision-making:
Though currently this effort is mainly an anesthesia-led effort, I wonder if this could provide the infrastructure for stronger perioperative protocols and goal-directed post-surgical medical management.
Value-based Vascular Surgery
Inspired by patients I’ve seen working under Dr. Alan Benvenisty this month and brainstorming sessions I’ve had with a long-standing physician-entrepreneur mentor from Stanford, Dr. Oliver Aalami, I looked deeper into a few ways that we could create more value-based vascular surgery care models.
In line with the Society of Vascular Surgery’s alternative payment model (APM) taskforce, I believe peripheral artery disease (PAD) holds the largest promise to be vascular surgery’s first value-based care model. Drawing on learnings from companies like Vori Health which offer digital health interventions for non-operative back pain, we could build virtualized supervised exercise therapy or smoking cessation counseling services that allow surgeons to better manage non-operative PAD. Of note, CMS already covers up to 36 sessions over 12 weeks so better integration of exercise therapists could be a low-hanging opportunity for vascular surgery clinics today.
Building on the success of the comprehensive joint replacement program, coordinated services that coordinate surgeons, home health agencies, physical therapy, to ultimately drive down perioperative and post-acute costs when surgery is indicated. As Dr. Duwayri and his colleagues highlight, the success of an APM for PAD will largely hinge on cost-effective post-discharge coordination and identifying opportunities to decrease length of stay in rehab facilities or creating more intensive but cost-effective options for patients to continue rehabilitation at home.
In terms of growth verticals, we know smoking is a large risk factor for symptomatic PAD and partnering closely with employers or employer wellness programs that already engage a disproportionate amount of patients who smoke can be a scalable way to grow this service. Partnering first with employers to develop the proper risk adjustment and cost benchmarking metrics to bring to a payer could be one way to overcome some of the current roadblocks in creating this APM model today.
Big thanks to Dr. Alan Benvenisty who was generous in his time teaching me and many others - it’s no surprise why he has inspired many of my classmates and predecessors to pursue surgery. Extremely dedicated to his patients and well-liked by everyone who has the pleasure of working with him. Thanks also to Dr. Daniel Han, Dr. Sanghyun Kim, and Dr. Suarez-Rodriguez who were exceptional teachers while in the OR and gave me glimpses of trauma, colorectal, bariatric, and endovascular surgery. For other Mt Sinai students interested in surgery or not, consider rotating at Mt Sinai West/Morningside - Dr. Susan Lerner and Dr. Adam Korayem have done great work in providing a supportive learning environment. Finally, my time on surgery wouldn’t have been as the same without the more than accommodating and encouraging surgery and vascular surgery residents I worked every day with - shout-out to Quinn, Dean, Joe, and Mike in particular!
Hope to continue posting more of these learnings and snapshots from my time on the wards as I continue through third year - subscribe above and let me know what you’d be most interested in hearing more about!




